The SanvaadGarh Desk
India’s flagship health insurance scheme Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (PM-JAY) was launched in 2018 with a promise: “Healthcare for all.” But seven years later, that promise stands hollow in the corridors of many hospitals where the poor are turned away, denied, or deceived.
SanvaadGarh’s month-long investigation across Uttar Pradesh, Bihar, and Madhya Pradesh found a disturbing pattern: fake hospital claims, ghost patients, inflated bills, and a systemic failure of oversight that’s bleeding both lives and public money.
The Mirage of “Free” Healthcare
Take the case of Rajkumar Paswan from Darbhanga, Bihar. Admitted for gallbladder surgery under Ayushman Bharat, he was discharged midway when his family couldn’t pay ₹15,000 “extra service charges.” The hospital later claimed ₹30,000 from the scheme marked “successfully treated.”
In Lucknow, Uttar Pradesh, the SanvaadGarh team found hospitals billing the government for “free treatment” of patients who had died months earlier. In one instance, a facility had filed claims for over 200 cataract surgeries in a single day, a physical impossibility.
RTI data from the National Health Authority (NHA) shows that over ₹1,100 crore worth of fraudulent or suspicious claims have been flagged since 2021, but only 27% of those have been recovered. Most states have yet to file criminal cases.
A former NHA official, speaking on condition of anonymity, said:
“The fraud isn’t limited to private hospitals, government hospitals are in on it too. They claim reimbursements for patients who never existed. It’s a system built on paperwork, not people.”
When Denial Becomes Death
In Shivpuri, Madhya Pradesh, Kusum Bai, a 58-year-old widow, was refused admission for chest pain because her card didn’t “reflect the updated family ID.” She died at home waiting for the local Ayushman Mitra to “fix” her biometric error.
Across India, stories like hers are piling up. A 2024 study by Oxfam India found that 47% of eligible beneficiaries were denied treatment due to technical or administrative barriers, including biometric mismatches, inactive e-cards, or hospitals simply refusing Ayushman cases.
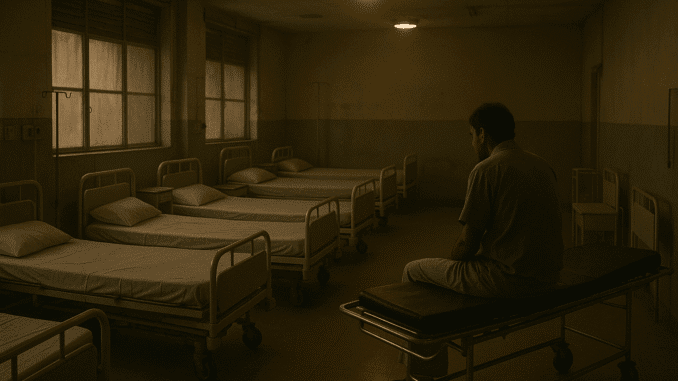
For millions, Ayushman Bharat exists only on banners not in hospital beds.
The Ghost in the Database
At the heart of the scam lies India’s growing digital blind spot: data-based welfare without data-based accountability.
Hospitals exploit loopholes in the digital claims system, registering patients with minor ailments for high-value procedures, or duplicating IDs to file multiple claims.
A data analyst who reviewed claim patterns for SanvaadGarh noted:
“In some districts, claims for major surgeries exceed the actual number of hospital beds. The algorithm doesn’t question, it just approves.”
Meanwhile, whistleblowers inside NHA’s partner agencies say there’s political pressure to keep “success figures” high for PR purposes.
The Accountability Vacuum
Despite multiple CAG audits warning of “high vulnerability to misuse,” there have been no large-scale prosecutions of fraudulent hospitals. State health departments quietly blacklist some facilities, but many re-register under new names.
Public outrage remains muted because the poor, who suffer most, have no platform to speak.
Ayushman Bharat was meant to heal inequality; instead, it’s become a mirror of it.
The Question That Lingers
In the end, the scheme’s failure isn’t technological, it’s moral.
A nation that prides itself on digital progress still allows its poorest citizens to die waiting for “free treatment.”
Ayushman Bharat promised dignity in illness. What it delivered was denial in disguise.





Be the first to comment